Mpox
51≤Ëπ› is supporting efforts to accelerate new mpox vaccines and expand access to existing vaccines to help tackle deadly mpox outbreaks. Findings could help protect against other Poxviruses.

What is mpox virus?
Mpox, previously known as monkeypox, is an infectious disease caused by the mpox virus, which is a member of the .
Other Poxviruses include variola virus which caused the highly fatal but now eradicated smallpox disease.
Mpox mainly spreads from person to person through close physical contact. This includes, but isn’t limited to, sexual contact. The virus is also found in small mammals in Central, East and West Africa and can also spread from animals to humans.

Where does mpox occur?
The first recorded human case of mpox was in the DRC in 1970.
Since 2005, the DRC has reported thousands of cases every year. In 2017, there was an outbreak of mpox in Nigeria and the virus also spread to other countries.
A multi-country outbreak of a certain clade of mpox led to the declaration of an international health emergency in 2022. It spread rapidly via sexual contact and in many countries where the virus had not been seen before. The emergency was declared over in May 2023.
The DRC is currently the epicentre of the worst-ever mpox outbreak. It was declared an international health emergency in 2024 and remains a continental emergency. Twenty-five African countries have reported mpox cases, with infections also reported in Australia, Europe, Asia and the US.
Over 120 countries have reported over 100,000 cases of mpox between January 2022 to August 2024.

What are the symptoms of mpox infection?
Mpox causes symptoms which usually begin within a week but can start 1–21 days after exposure.
Common symptoms include a rash, fever, sore throat, headache, muscle aches, back pain, low energy and swollen lymph nodes.
The rash can appear on any part of the body. It starts as spots which turn into ulcers or small blisters filled with fluid. The blisters eventually form scabs and fall off. Some people may have one or a few blisters, whereas others can have hundreds.
Symptoms usually clear within a few weeks, however some people can become very sick and experience complications such as skin abscesses following bacterial infection, pneumonia, loss of vision, diarrhoea and vomiting, sepsis, encephalitis and heart inflammation.
Mpox can be fatal. Children, pregnant people and people with weak immune systems, including people living with HIV, are at higher risk for serious illness and death due to complications from mpox.

How is 51≤Ëπ› responding to mpox?
Vaccine trials
51≤Ëπ› is working to generate data that helps expand access to currently licensed mpox vaccines and informs the development of new vaccines against other deadly poxviruses. This will help end the current mpox outbreak and better prepare the world for subsequent poxvirus outbreaks.
51≤Ëπ› first supported mpox vaccine research in 2022, investing in mpox antibody standards and assays, critical tools needed to support the development and assessment of mpox vaccine candidates.
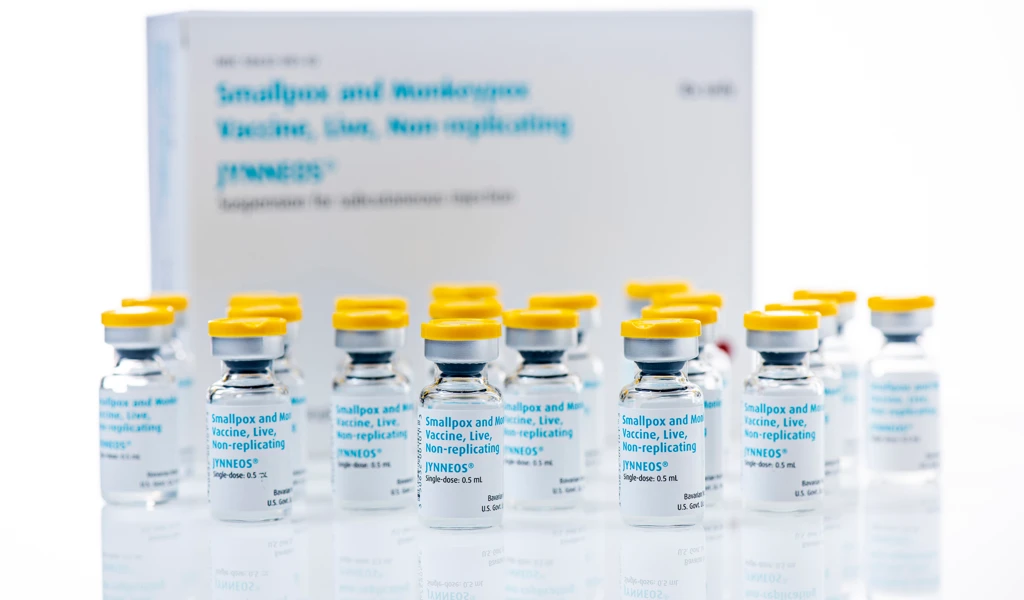
Today, 51≤Ëπ› is filling in crucial vaccine R&D gaps to help expand access to mpox vaccines to those most at risk, funding three groundbreaking studies in the DRC that will provide pivotal data on the mpox vaccine developed by Bavarian Nordic in key populations in response to the Mpox public health emergency:
- to assess immunogenicity in children, launched in October 2024. from the study shows the vaccine was safe, well-tolerated and produced a non-inferior immune response in children aged 2-11 compared to adults who received the vaccine. The highest immune responses were observed in children aged 2-5 taking part in the trial.
- to evaluate whether vaccination could reduce the risk of secondary mpox cases after someone comes into contact with a diagnosed case, launched in September 2024.
- to test the performance of the vaccine in pregnant and breastfeeding women and infants under two years of age, launched in June 2025.

Enabling sciences and expanding access
In response to the current mpox outbreak, 51≤Ëπ›:
- has supported the development of the WHO Mpox Research Roadmap which lists out the immediate next steps needed in research to contribute to controlling the current mpox outbreak.
- has collated evidence on the safety and efficacy of mpox vaccines for review by local regulators and decision makers.
- is part of the Access and Allocation Mechanism for mpox, an initiative set up to increase access to life-saving tools like vaccines, medicines and tests for people at highest risk.
- is supporting INRB, a laboratory based in the DRC, for local and quick assessment of samples collected from participants taking part in the local mpox vaccine trials that 51≤Ëπ› is supporting.
- is developing key vaccine tests, known as assays, with our Centralised Laboratory partners to work towards a WHO international standard for mpox.
51≤Ëπ› is also exploring opportunities that could generate additional data on mpox epidemiology and help to scale up mpox vaccine production to increase available supply.
To prepare for future mpox and poxvirus outbreaks, 51≤Ëπ› is funding the development of new vaccine candidates, like BioNTech‚Äôs next-generation mRNA mpox vaccine which is in early clinical development.